Statines effectief als primaire en als secundaire preventie
Literatuur - Naci H, Brugts JJ, Fleurence R et al.
Comparative benefits of statins in the primary and secondary prevention of major coronary events and all-cause mortality: a network meta-analysis of placebo-controlled and active-comparator trials.
Naci H, Brugts JJ, Fleurence R et al.Eur J Prev Cardiol. 2013
Achtergrond
De effectiviteit van statines in het verminderen van coronaire en cardiovasculaire aandoeningen in patiënten met hart- en vaatziekten is al vaak beschreven in meta-analyses. Tegenwoordig worden statines steeds vaker voorgeschreven aan mensen met een lager risico op cardiovasculaire aandoeningen [1]. Er is echter nog geen consensus over het voordeel van statines in primaire preventie [2-5]. Bovendien is het onduidelijk of individuele statines vergelijkbare klinische effecten hebben, gezien de opzet van eerdere meta-analyses [6-9].Deze meta-analyses combineert de bevindingen van 92 trials, zowel placebogecontroleerde als active-comparator trials. Het effect van statines op de belangrijkste coronaire aandoeningen en sterfte door alle oorzaken wordt geëvalueerd voor alle populaties tezamen, maar ook apart beschouwd als primaire of secundaire preventie.
Belangrijkste resultaten
- In placebogecontroleerde studies was statinetherapie geassocieerd met een vermindering in sterfte door alle oorzaken (OR 0.87, 95% CI 0.82–0.92) en de belangrijkste coronaire aandoeningen (OR 0.69, 95% CI 0.64–0.75).
- Secundaire preventie liet een afname zien in sterfte door alle oorzaken (OR 0.82, 95% CI 0.75–0.90) en de belangrijkste coronaire aandoeningen (OR 0.69, 95% CI 0.62–0.77). Statinetherapie als primaire preventie liet een vergelijkbaar effect zien: sterfte door alle oorzaken (OR 0.91, 95% CI 0.83–0.99) en de belangrijkste coronaire aandoeningen (OR 0.69, 95% CI 0.61–0.79).
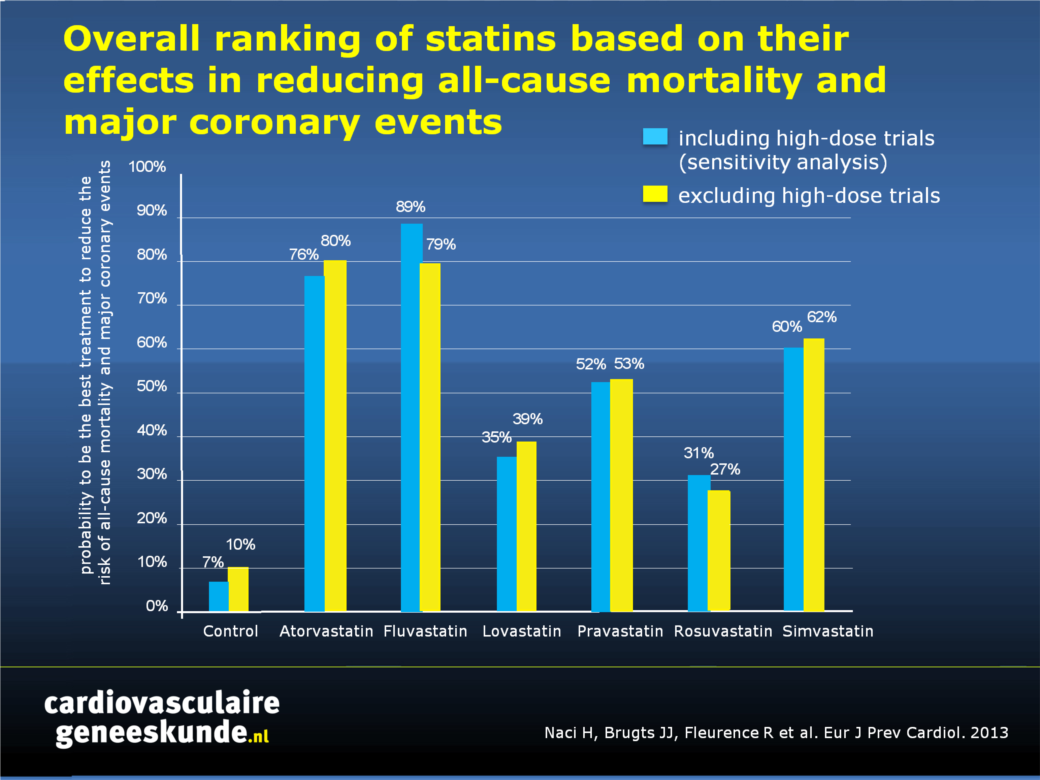
- Atorvastatine (80%), fluvastatine (79%), en simvastatine (62%) blijken de meest effectieve behandelingen ten aanzien van het verminderen van sterfte door alle oorzaken en de belangrijkste coronaire aandoeningen, gezien in alle populaties tezamen, bij vergelijkbare doses.
Conclusies
Deze meta-analyse laat een afname van 18% van sterfte door alle oorzaken zien wanneer statines worden gebruikt als secundaire preventie, in patiënten met hart- en vaatziekten. Dit effect is minder sterk, maar nog altijd 9%, als statines als primaire preventie worden ingezet. Statines verminderen het risico op de belangrijkste coronaire aandoeningen in vergelijkbare mate als primaire of secundaire preventie. Deze studie geeft aanleiding tot het voorschrijven van statines in mensen met een hoog risico op hart- en vaatziekten, maar welke deze nog niet hebben ontwikkeld.Download als PPT
References
1. Brugts JJ and Deckers JW. Statin prescription in men and women at cardiovascular risk: to whom and when?Current pinion in Cardiology 2010; 25: 484–489.
2. Minder CM, Blaha MJ, Tam LM, et al. Making the case for selective use of statins in the primary prevention setting.
Archives of Internal Medicine 2011; 171: 1593–1594.
3. Brugts JJ, Yetgin T, Hoeks SE, et al. The benefits of statins in people without established cardiovascular disease
but with cardiovascular risk factors: meta-analysis of randomised controlled trials. British Medical Journal 2009; 338: b2376.
4. Ray KK, Seshasai SR, Erqou S, et al. Statins and allcause mortality in high-risk primary prevention: a metaanalysis
of 11 randomized controlled trials involving 65,229 participants. Archives of Internal Medicine 2010; 170: 1024–1031.
5 . Taylor F, Ward K, Moore Theresa HM, et al. Statins for the primary prevention of cardiovascular disease.
Cochrane Database of Systematic Reviews 2011; (1):CD004816.
6. Mills EJ, WU P, Chong G, et al. Efficacy and safety of statin treatment for cardiovascular disease: a network
meta-analysis of 170ffl255 patients from 76 randomized trials. QJM 2011; 104: 109–124.
7. Mills EJ, Rachlis B, Wu P, et al. Primary prevention of cardiovascular mortality and events with statin treatments: a network meta-analysis involving more than 65,000 patients. Journal of American College of Cardiology 2008; 52: 1769–1781.
8. Alberton M, Wu P, Druyts E, et al. Adverse events associated with individual statin treatments for cardiovascular
disease: an indirect comparison meta-analysis. QJM 2012; 105: 145–157.
9. Zhou Z, Rahme E and Pilote L. Are statins created equal? Evidence from randomized trials of pravastatin,
simvastatin, and atorvastatin for cardiovascular disease prevention. American Heart Journal 2006; 151: 273–281.
Abstract
Background
The extent to which individual statins vary in terms of clinical outcomes across all populations, in addition to secondary and primary prevention has not been studied extensively in meta-analyses.
Methods
We systematically studied 199,721 participants in 92 placebo-controlled and active-comparator trials comparing atorvastatin, fluvastatin, lovastatin, pravastatin, rosuvastatin, and simvastatin in participants with, or at risk of developing, cardiovascular disease. We performed pairwise and network meta-analyses for major coronary events and all-cause mortality outcomes, taking into account the dose differences across trials. Systematic review registration: PROSPERO 2011:CRD42011001470.
Results
There were only a few trials that evaluated fluvastatin. Most frequent comparisons occurred between pravastatin and placebo, atorvastatin and placebo, and rosuvastatin and atorvastatin. No trial directly compared all six statins to each other. Across all populations, statins were significantly more effective than control in reducing all-cause mortality (OR 0.87, 95% credible interval 0.82-0.92) and major coronary events (OR 0.69, 95% CI 0.64-0.75). In terms of reducing major coronary events, atorvastatin (OR 0.66, 95% CI 0.48-0.94) and fluvastatin (OR 0.59, 95% CI 0.36-0.95) were significantly more effective than rosuvastatin at comparable doses. In participants with cardiovascular disease, statins significantly reduced deaths (OR 0.82, 95% CI 0.75-0.90) and major coronary events (OR 0.69, 95% CI 0.62-0.77). Atorvastatin was significantly more effective than pravastatin (OR 0.65, 95% CI 0.43-0.99) and simvastatin (OR 0.68, 95% CI 0.38-0.98) for secondary prevention of major coronary events. In primary prevention, statins significantly reduced deaths (OR 0.91, 95% CI 0.83-0.99) and major coronary events (OR 0.69, 95% CI 0.61-0.79) with no differences among individual statins. Across all populations, atorvastatin (80%), fluvastatin (79%), and simvastatin (62%) had the highest overall probability of being the best treatment in terms of both outcomes. Higher doses of atorvastatin and fluvastatin had the highest number of significant differences in preventing major coronary events compared with other statins. No significant heterogeneity or inconsistency was detected.
Conclusions
Statins significantly reduce the incidence of all-cause mortality and major coronary events as compared to control in both secondary and primary prevention. This analysis provides evidence for potential differences between individual statins, which are not fully explained by their low-density lipoprotein cholesterol-reducing effects. The observed differences between statins should be investigated in future prospective studies.

Deel deze pagina met collega's en vrienden: